Fallopian tube cancer
| Fallopian tube cancer | |
|---|---|
| Other names: Malignant neoplasm of unspecified fallopian tube[1] | |
  | |
| Specialty | Oncology, gynecology |
| Symptoms | Early: Vague, none Later: Abnormal vaginal bleeding, abdominal distension, blood stained watery vaginal discharge, pelvic pain, dyspareunia, loss of appetite, weight loss, feel full, tiredness[2] |
| Risk factors | Family history of ovarian cancer, breast cancer[3] BRCA1 and BRCA2 mutations[4] |
| Diagnostic method |
|
| Differential diagnosis | Ovarian cancer, peritoneal cancer[4] |
| Treatment | Surgery[3] |
| Medication | Chemotherapy: carboplatin, paclitaxel[3] |
| Prognosis | Five-year survival rate c 65% (varies between 30% to 92% depending on stage)[4][5] |
| Frequency | Underestimated 0.41 per 100,000 cases per year[4] |
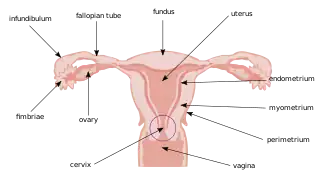
Fallopian tube cancer (FTC), also known as tubal cancer, is cancer that originates in the fallopian tube.[1][4] In the early stages, symptoms maybe absent or vague.[2] Other symptoms may include abnormal vaginal bleeding, blood stained watery vaginal discharge, tiredness, pelvic pain, dyspareunia, or abdominal distension.[2][3] An affected person may feel full or have weight loss.[4] It may be found at an early stage when removing the tubes and ovaries as a preventive measure.[4]
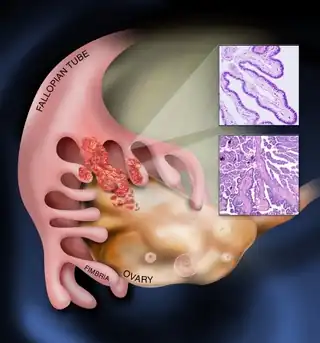
Along with primary ovarian and peritoneal cancer, fallopian tube cancer is grouped under epithelial ovarian cancers; cancers of the ovary that originate from a fallopian tube precursor.[5][6] Most high grade serous type ovarian cancers are believed to originate from the precursor serous tubal intraepithelial carcinoma in the fallopian tubes.[7][8] Risk factors include a family history of ovarian or breast cancer, particularly if carriers of mutations in the genes BRCA1 or BRCA2.[4][3]
Diagnosis is by blood tests, medical imaging, and pathologic assessment of fallopian tissue.[4] Blood tests include Ca-125 and CBC.[4] Imaging includes transvaginal and abdominal ultrasound, CT scan, and MRI.[3] Pathologic assessment may include microscopic examination of the fallopian tube fimbriae.[4] Ovarian and peritoneal cancers may present in a similar way.[4] Treatment is similar to that of ovarian cancer.[3] This generally involves surgery to remove the tumor, uterus, ovaries, and visible lymph nodes.[4] This is typically followed by chemotherapy such as carboplatin and paclitaxel.[3] These may require being given by injection into vein or into peritoneum.[5] There is no role for radiotherapy.[4] Five-year survival rate is around 65%, though may range from 30% to 92% depending on stage at diagnosis and the amount of tumor remaining after surgery.[4][5]
FTC was initially thought to be rare, at around 0.41 per 100,000 cases per year, a figure now felt to be underestimated.[4][7] In the United States, FTC, ovarian cancer and primary peritoneal cancer, together, account for around 2.5% of all new female cancers; 22,000 per year or 11.6 per 100,000 females per year.[5] The first descriptions of FTC were made by Renaud in 1847 and Ernst Gottlob Orthmann in 1888.[9]
Signs and symptoms
In the early stages of tubal cancer, symptoms maybe absent or vague.[4][3] Other symptoms may include abnormal vaginal bleeding, blood stained watery vaginal discharge, pelvic pain, dyspareunia, or abdominal distension.[3] An affected person may feel full or have weight loss.[4]
FTC may be found at an early stage when removing the tubes and ovaries as a preventive measure.[4] A pelvic mass may be detected on a routine gynecologic examination.[3]
Pathology
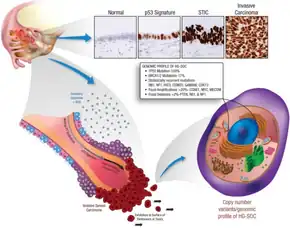
The most common cancer type within this disease is adenocarcinoma; in the largest series of 3,051 cases as reported by Stewart et al. 88% of cases fell into this category.[10] According to their study, half of the cases were poorly differentiated, 89% unilateral, and the distribution showed a third each with local disease only, with regional disease only, and with distant extensions. Rarer forms of tubal neoplasm include leiomyosarcoma, and transitional cell carcinoma.
Diagnosis
Diagnosis is by blood tests, medical imaging, and pathologic assessment of fallopian tissue.[4] Blood tests include Ca-125 and CBC.[4] Imaging includes transvaginal and abdominal ultrasound, CT scan, and MRI.[3] Pathologic assessment may include SEE-FIM Protocol.[4] Ovarian and peritoneal cancers may present in a similar way.[4] It may be found at an early stage when removing the tubes and ovaries as a preventive measure.[4]
Staging
| Stage | Definition |
|---|---|
| Stage 0 | Carcinoma in situ[4] |
| Stage I | Growth limited to fallopian tubes[4] |
| Stage II | Growth involving one or both fallopian tubes with extension to pelvis[4] |
| Stage III | Tumor involving one or both fallopian tubes with spread outside pelvis[4] |
| Stage IV | Growth involving one or more fallopian tubes with distant metastases[4] |
Treatment
The initial approach to tubal cancer is generally surgical, and similar to that of ovarian cancer.[4] As the lesion will spread first to the adjacent uterus and ovary, a total abdominal hysterectomy is an essential part of this approach, removing the ovaries, the tubes, and the uterus with the cervix. Also, peritoneal washings are taken, the omentum is removed, and pelvic and paraaortic lymph nodes are sampled. Staging at the time of surgery and pathological findings will determine further steps. In advanced cases when the cancer has spread to other organs and cannot be completely removed, cytoreductive surgery is used to lessen the tumor burden for subsequent treatments. Surgical treatments are typically followed by adjuvant, usually platinum-based, chemotherapy.[11][12]
Prognosis
Five-year survival rate is around 65%, though may range from 30% to 92% depending on stage at diagnosis and the amount of tumor remaining after surgery.[4][5]
Frequency
FTC was initially thought to be rare, at around 0.41 per 100,000 cases per year, a figure now felt to be underestimated.[4][7] In the United States, FTC, ovarian cancer and primary peritoneal cancer, together, account for around 2.5% of all new female cancers; 22,000 per year or 11.6 per 100,000 females per year.[5]
Demographic distribution is similar to that of ovarian cancer, and the highest incidence is found in white, non-Hispanic women aged 60–79.[10]
History
The first descriptions were made by Renaud in 1847 and Ernst Gottlob Orthmann in 1888.[9]
See also
References
- 1 2 WHO Classification of Tumours Editorial Board, ed. (2020). "4. Tumours of the fallopian tube: introduction". Female genital tumours: WHO Classification of Tumours. Vol. 4 (5th ed.). Lyon (France): International Agency for Research on Cancer. p. 216. ISBN 978-92-832-4504-9. Archived from the original on 2022-06-17. Retrieved 2024-03-30.
- 1 2 3 "Ovarian, Fallopian Tube, and Peritoneal Cancer - Symptoms and Signs". Cancer.Net. 25 June 2012. Archived from the original on 5 January 2024. Retrieved 12 May 2024.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 "Fallopian tube cancer". www.cancerresearchuk.org. Archived from the original on 30 March 2024. Retrieved 30 March 2024.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 Ferri, Fred F. (2024). "Fallopian tube cancer". Ferri's Clinical Advisor 2024. Philadelphia: Elsevier. p. 568.e5. ISBN 978-0-323-75576-4. Archived from the original on 2024-04-22. Retrieved 2024-04-22.
- 1 2 3 4 5 6 7 Stasenko, Marina; Fillipova, Olga; Tew, William P. (July 2019). "Fallopian Tube Carcinoma". Journal of Oncology Practice. 15 (7): 375–382. doi:10.1200/JOP.18.00662. ISSN 1554-7477. Archived from the original on 2024-03-30. Retrieved 2024-03-30.
- ↑ Armstrong, Deborak K. (2020). "189. Gynaecologic cancers". In Goldman, Lee; Schafer, Andrew I. (eds.). Goldman-Cecil Medicine. Vol. 1 (26th ed.). Philadelphia: Elsevier. pp. 1327–1335. ISBN 978-0-323-55087-1. Archived from the original on 2023-01-14. Retrieved 2024-05-06.
- 1 2 3 Rashid, Sameera; Arafah, Maria A.; Akhtar, Mohammed (1 May 2022). "The Many Faces of Serous Neoplasms and Related Lesions of the Female Pelvis: A Review". Advances in Anatomic Pathology. 29 (3): 154–167. doi:10.1097/PAP.0000000000000334. ISSN 1533-4031. Archived from the original on 29 July 2022. Retrieved 29 July 2022.
- ↑ "Ovarian, Fallopian Tube, and Peritoneal Cancer - Introduction". Cancer.Net. 25 June 2012. Archived from the original on 18 February 2024. Retrieved 31 March 2024.
- 1 2 Laury, Anna; Huang, Eric C.; Crum, Christopher P.; Hecht, Jonathan (2013). "7. Peritoneal and tubal serous carcinoma". In Deligdisch, Liane; Kase, Nathan G.; Cohen, Carmel J. (eds.). Altchek's Diagnosis and Management of Ovarian Disorders (3rd ed.). Cambridge University Press. pp. 111–120. ISBN 978-1-107-01281-3. Archived from the original on 2024-05-03. Retrieved 2024-05-03.
- 1 2 Stewart SL, Wike JM, Foster SL, Michaud F (2007). "The incidence of primary fallopian tube cancer in the United States". Gynecol. Oncol. 107 (3): 392–7. doi:10.1016/j.ygyno.2007.09.018. PMID 17961642. Archived from the original on 2019-11-17. Retrieved 2021-12-26.
- ↑ Liapis A, Bakalianou K, Mpotsa E, Salakos N, Fotiou S, Kondi-Paffiti A (2008). "Fallopian tube malignancies: A retrospective clinical pathological study of 17 cases". J Obstet Gynaecol. 28 (1): 93–5. doi:10.1080/01443610701811894. PMID 18259909. S2CID 5351886.
- ↑ Takeshima N, Hasumi K (2000). "Treatment of fallopian tube cancer. Review of the literature". Arch Gynecol Obstet. 264 (1): 13–9. doi:10.1007/pl00007475. PMID 10985612. S2CID 34114333.
External links
| Classification | |
|---|---|
| External resources |
|